Wrong Breastmilk to My Baby in the NICU - St. Joseph's Health Centre, Toronto, Ontario

Unity Health Toronto
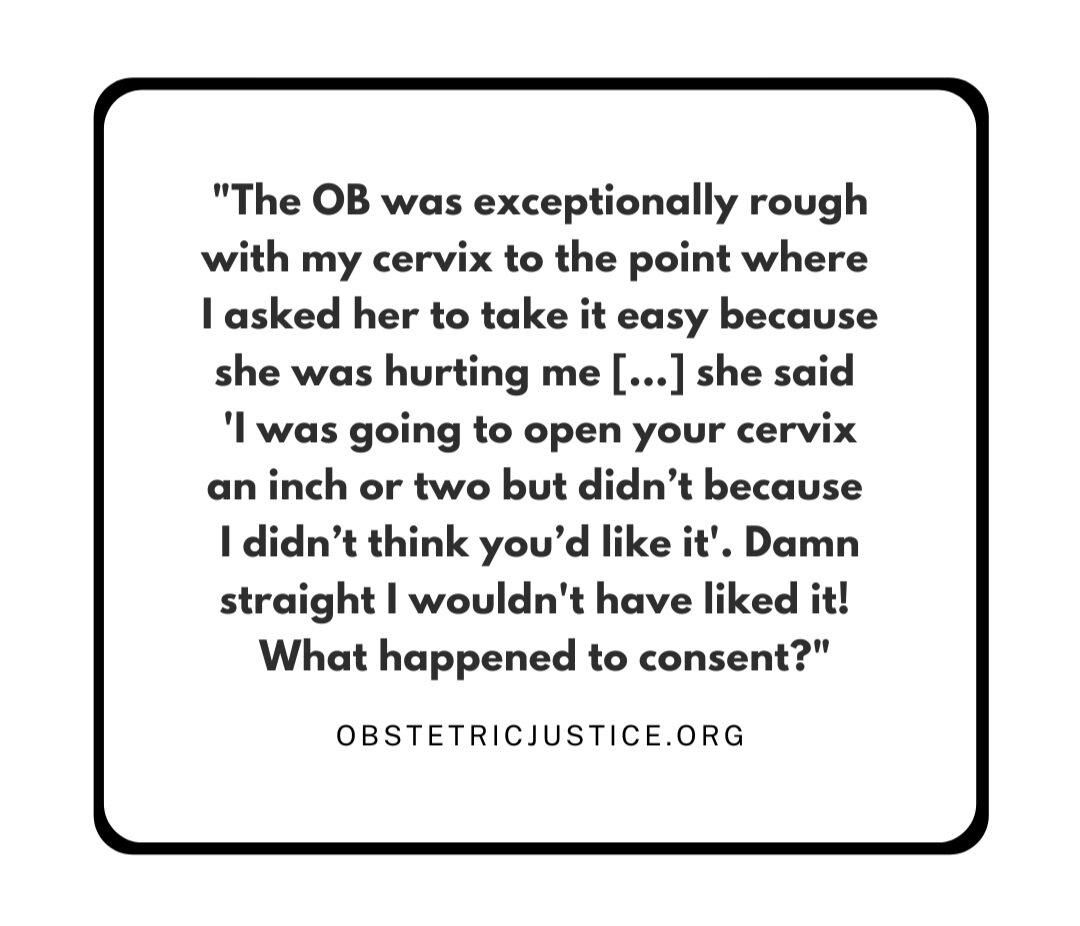

The Obstetric Justice Project

The Obstetric Justice Project

Submitted by AB